12 YEARS ANNIVERSARY
Celebrating 12 Years of Healing

Hridaya Care Heart Institute was founded and is run by Dr. Gopalakrishnan A. Pillai M.D., Ph.D. (Cardiovascular Surgery), a cardiovascular surgeon with over 40 years of experience in cardiology and cardiac surgery with over 10,000 heart surgeries behind him.

Dr. G.A. Pillai also works with Amrita Institute of Medical Sciences & Research Centre (AIMS, Kochi) - (Visiting consultant) & Sri Ramachandra Medical College & Research Institute (Visiting associate professor)
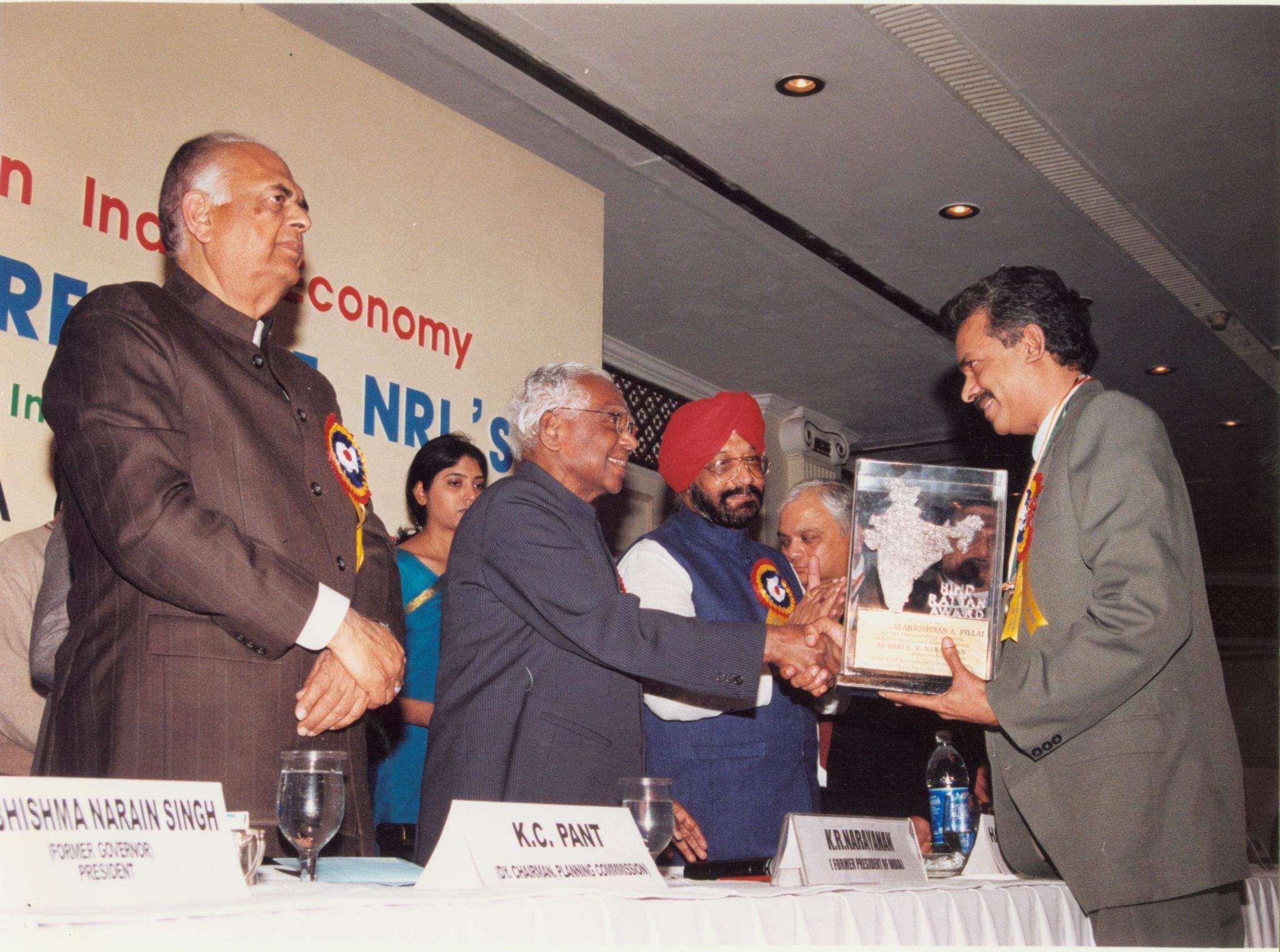
PRESIDENT'S AWARD : He is also the recipient of the prestigious HIND RATTAN (Jewel of India) award from His Excellency K.R. Narayanan, President of India.
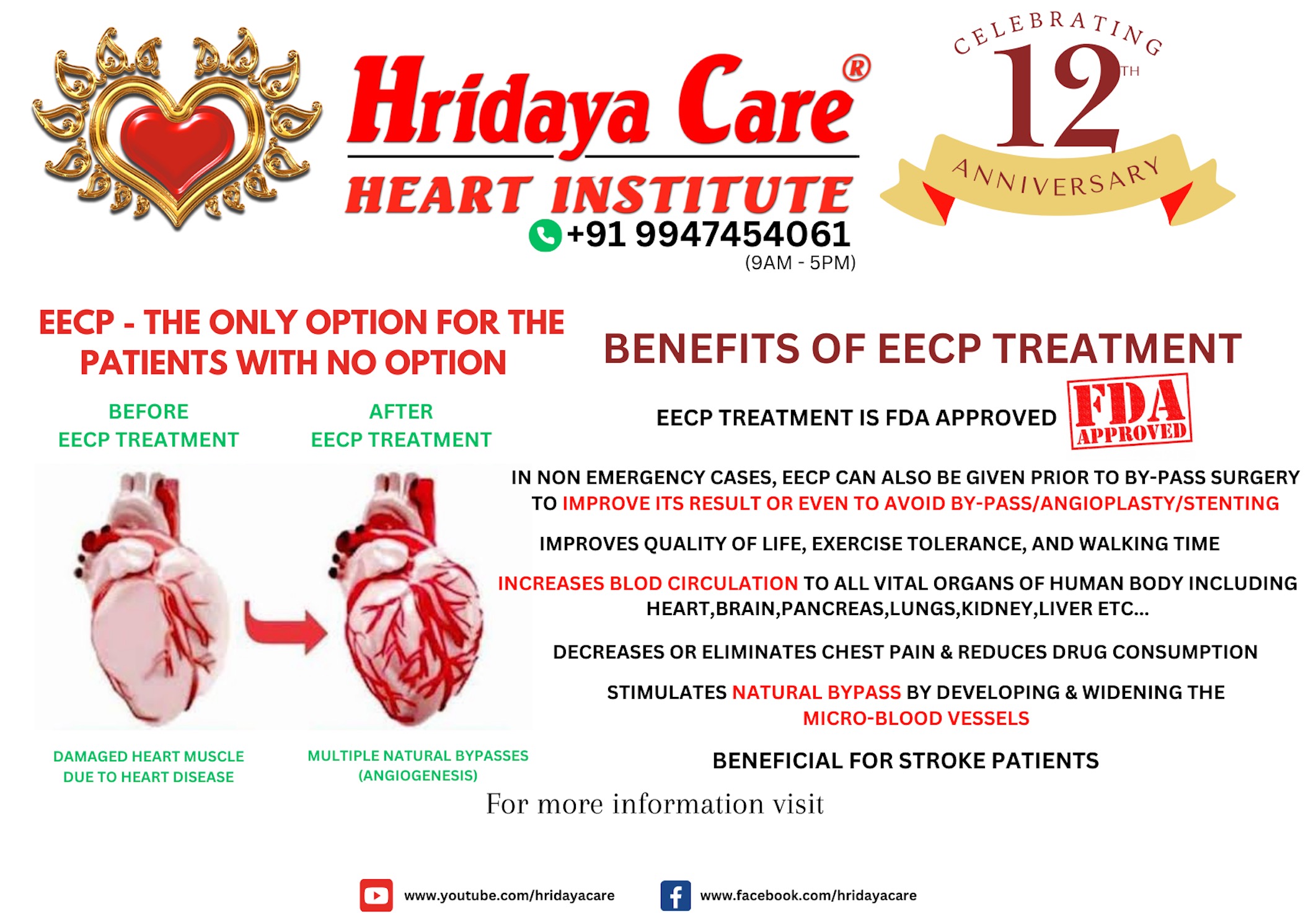
What is EECP Therapy?
EECP therapy, which stands for Enhanced External Counterpulsation therapy, is a non-invasive and non-pharmaceutical treatment option primarily used for individuals with cardiovascular conditions such as angina (chest pain) or heart failure. It involves the use of inflatable cuffs wrapped around the patient's calves, thighs, and buttocks, which are synchronized with the patient's cardiac cycle.
Benefits of EECP therapy include:
-
Angina relief
EECP therapy has been shown to reduce the frequency and severity of angina episodes in individuals with chronic stable angina.
-
Improved exercise tolerance
By enhancing blood flow and oxygen delivery, EECP therapy may help individuals tolerate physical activity with less discomfort and fatigue.
-
Quality of life improvement
: Reduced angina symptoms and improved exercise capacity can contribute to an overall improvement in an individual's quality of life.
-
Non-invasive and safe
: EECP therapy is a non-surgical and non-pharmaceutical treatment option. It is generally considered safe, with minimal side effects and a low risk of complications.
Other Benefits include:
-
Beneficial for patients who had a stroke
Neurological recovery: EECP therapy has been proposed as a potential adjunctive therapy for stroke rehabilitation. The enhanced blood flow and oxygen supply to the brain during treatment could potentially support the recovery of damaged brain tissue and aid in the rewiring of neural connections. However, further research is needed to establish the effectiveness of EECP specifically for stroke recovery.
- Lower extremity function: Stroke often leads to impaired motor function in the lower extremities. EECP therapy involves the application of external pressure to the lower extremities, which can improve blood flow, muscle function, and potentially contribute to enhanced mobility and strength in the legs.
- Cardiovascular fitness: Stroke survivors may experience reduced cardiovascular fitness due to limited mobility and physical activity. EECP therapy, by improving blood flow and exercise tolerance, could potentially support cardiovascular fitness and enable stroke patients to engage in physical activities with less discomfort.
- Overall well-being: Stroke recovery can be a challenging and complex process that affects not only physical function but also emotional well-being. EECP therapy, by promoting better circulation and potentially reducing symptoms such as fatigue, may contribute to an improved sense of well-being and overall quality of life for stroke patients.
-
Can help with certain cases of diabetes
EECP (Enhanced External Counterpulsation) therapy can be beneficial for individuals with diabetes,
In some cases diabetes is caused due to poor blood circulation in the pancreas. EECP helps improve the circulation and intern improve the functioning of the pancreas
In our experience, we were able to control blood sugar levels of many patients, and some were even able to discontinue the use of insulin.
Managing diabetes can be a lifelong challenge, but with the right care, dedication, and advanced therapies, we strive to provide you with the best possible outcomes. The positive impact of EECP therapy on diabetes management has been nothing short of remarkable. While EECP therapy primarily targets cardiovascular complications associated with diabetes, it has shown some additional metabolic benefits, leading to improved glucose control and insulin sensitivity in certain individuals.
-
Improves circulation to all organs
- Enhanced endothelial function: EECP therapy has been shown to improve endothelial function, which is crucial for maintaining healthy blood vessels. By promoting the release of nitric oxide and reducing inflammation, EECP can enhance the dilation and flexibility of blood vessels throughout the body, leading to improved blood flow and circulation to different organs.
- Collateral vessel development: EECP therapy has the potential to stimulate the formation of collateral blood vessels, which are additional pathways that can bypass blocked or narrowed arteries. These collateral vessels can help deliver oxygenated blood to organs and tissues that may have reduced blood flow due to underlying conditions such as peripheral artery disease (PAD).
- Improved microcirculation: Microcirculation refers to the flow of blood through the smallest blood vessels, including capillaries. EECP therapy, by enhancing overall blood flow and increasing the pumping action of the heart, may positively impact microcirculation and ensure adequate blood supply to various organs and tissues.
- Organ-specific benefits: Although the primary focus of EECP is on the cardiovascular system, improved circulation can have positive effects on organ function. Adequate blood flow ensures oxygen and nutrient supply to organs, allowing them to function optimally. Enhanced circulation may benefit organs such as the kidneys, liver, brain, and muscles by improving their oxygenation and nutrient delivery.

Contact details
Address
Periyar Place, Desom - Chowra road, Desom, Aluva, Kerala 683102
Email
MD@hridayacare.com
drgapillai@gmail.com
